Skip to content
Venous Ulcers Treatment Advanced Wound Care Plano TX – Dr. Hina Rizvi M.D, C.W.Sadmin2021-11-18T17:49:45+00:00
Venous Ulcers
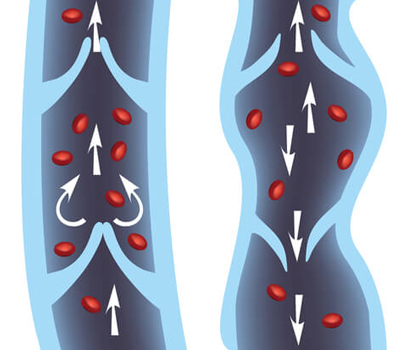
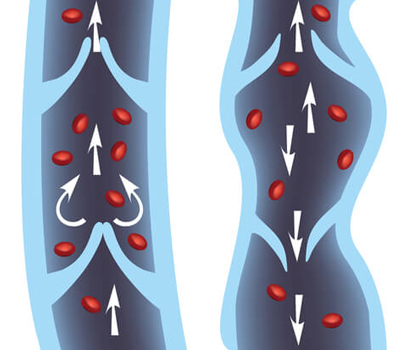
- Chronic venous disease is a common disorder that affects the veins of the legs. These veins carry blood from the legs to the heart. Normal veins have a series of valves that open and close to direct blood flow from the surface of the legs to the deep veins and back to the heart; the valves also control the pressure in smaller veins on the legs’ surface
 If the valves within the veins fail to work properly, blood can flow backwards in the veins and pool in the legs. The pooled blood can increase pressure in the veins.
If the valves within the veins fail to work properly, blood can flow backwards in the veins and pool in the legs. The pooled blood can increase pressure in the veins.- This can cause problems that are mild (such as leg heaviness, aching, dilated or unsightly veins) or severe (such as swelling, skin color changes, skin rash on the leg, recurrent skin infections and chronic ulcers).
- People who develop these more severe symptoms are said to have chronic venous insufficiency.
- Any problem that increases pressure in the veins in the legs can stretch the veins. This can damage the valves, which leads to even higher pressures and worsened vein function, and can eventually lead to chronic venous disease.
- A clot inside a vein can increase the pressure in the vein. A clot will block blood flow through the vein and cause pressure to build up. Often this causes permanent damage to the vein or valves, even after the clot has dissolved.
- Leg Injury or surgery that blocks the flow of blood through a vein can increase pressure
- Excess weight or weight gain – The added weight of pregnancy or obesity can increase pressure in the veins of the legs, and damage the veins and valves
- Prolonged standing or sitting without walking can decrease the movement of blood out of the legs and lead to increased pressure in the veins and pooling of blood. That’s because the muscles in the legs play an important role in the circulation of blood, acting as a pump to move blood from the legs back to the heart.
- Chronic venous disease can cause painless widened veins, skin irritation, skin rash, skin discoloration, itching, swelling, and skin ulcers.
- The legs may feel heavy, tired, or achy, usually at the end of the day or after prolonged standing.
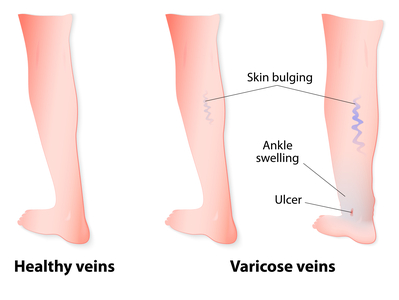
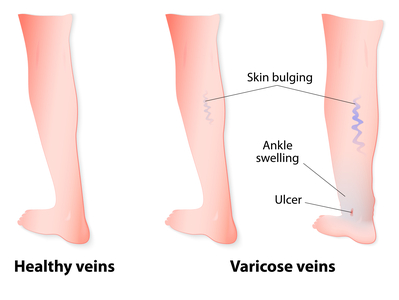
- The most frequent feature of venous disease is widening (dilation) of the veins. Dilated veins may appear as thin blue flares, often called spider veins, or much wider, twisted veins, called varicose veins that bulge on the surface.
- Long-standing chronic venous disease can cause swelling (edema) in the ankles and lower legs. Sometimes this swelling is evident only at the end of the day; other times it is present all the time.
- The area around the ankle bones is often the first place that swelling is seen.
- Pooling of blood and increased pressure in the veins can cause the skin to become red, and over months to years, the skin may become tan or a reddish-brown color. Often, the skin changes are initially noticeable around the ankle, but frequently occur over the shins and on the foot.
- Pooling of blood in the legs often causes the skin to become irritated and inflamed. This can cause redness, itching, dryness, oozing fluid, scaling, open sores from scratching, and crusting or scabbing. Some people develop an area of intensely painful skin that turns red or brown, and is hard, and scar-like. This usually develops after many years of venous disease but can occur suddenly.
- Open, non healing sores caused by chronic venous disease are called venous ulcers. These are usually located low on the inner ankle but can occur on the outer ankle and in the shin area. Venous ulcers rarely occur above the knee. Venous ulcers that occur higher on the leg are often the result of an injury, or trauma such as from repeated scratching. More than one ulcer can occur at a time.
- Venous ulcers often begin as small sores but can expand to become quite large. Venous ulcers are usually painful, tender to touch, shallow, have a red appearance at the bottom, and may ooze or drain small to large amounts of fluid.
- Venous ulcers can take a long time (months or sometimes years) to heal. Healing is a gradual process and the resulting scar is usually shiny pink or red with distinct white marks. Venous ulcers can come back even after they heal.
- Doctors can diagnose chronic venous disease by examining a person and asking about symptoms of the disorder, such as the presence of varicose veins, swelling in the legs, skin changes, or skin ulcers. They often also do additional testing, such as an ultrasound, to look at vein valve function and to identify if the problem is located in the superficial veins or the deep veins
- Treatment of chronic venous disease is focused on reducing symptoms, such as swelling, treating skin problems, and preventing and treating open ulcers and wounds
- Simply elevating the legs above heart level for 30 minutes three or four times per day can reduce swelling and improve blood flow in the veins. Improving blood flow can speed healing of venous ulcers.
- Foot and ankle exercises are often recommended to reduce symptoms. Pointing the feet down and up (movement from the ankle) several times throughout the day can help to move blood from the legs and back to the heart. This may be especially helpful for people who sit or stand for long periods of time.
- Walking is a good exercise for the calf muscle pump. People with chronic venous disease who walk less than 10 minutes a day have a greater risk for developing venous ulcers than those who are more physically active.
- Most experts consider compression therapy to be an essential treatment for chronic venous disease. People with more severe symptoms, such as venous ulcers, often need treatment with compression bandages.
- Compression therapy gently compress the legs, and may improve blood flow in the veins by preventing backward flow of blood.
- People with moderate to severe disease, those on their feet a lot, and those with ulcers usually require prescription compression therapy.
- Intermittent pneumatic compression pumps — Standard compression stockings may be less effective or difficult to use if you are very overweight or have a lot of swelling. An alternative approach is the use of intermittent pneumatic compression (IPC) pumps
- People with severe symptoms, like ulcers, may need to be treated with compression bandages and dressings. They are applied on the leg by an experienced nurse or doctor. Topical medicines may be applied to the skin, and if ulcers are present, they may be covered with special dressings before compression bandages are put on.
- The bandages are usually changed once or twice a week and must stay dry. It must be kept dry while showering. If you have compression bandages and they get wet, you should contact your doctor to have them changed.
- Ulcers are usually covered with special dressings before putting on compression stockings or compression bandages. Dressings are important to help ulcers heal. They are used to absorb fluid oozing out of the wound, reduce pain, control odor, remove dead or infected cells, and help new skin cells to grow.
- There are several types of dressing material used for venous ulcers. The type and frequency of dressings is determined by the size of the ulcer, amount of drainage, and other factors.
- Variety of medications have been used for chronic venous disease and venous ulcers which can be prescribed by your wound physician. Antibiotics are only recommended when there is an infection.
- Skin irritation caused by chronic venous disease, called stasis dermatitis, usually gets better with the use of medications. Sometimes, a steroid cream or ointment is needed to help with itching and inflammation.
- Creams, ointments, anti-itch products, and scented lotions should be avoided because there is a risk of developing an allergic rash (contact dermatitis) from these products.
- Contact dermatitis is an allergic skin reaction that occurs when an irritating or allergy-producing substance touches the skin. The reaction can occur on the legs or other areas of the body. Contact dermatitis is common in people with chronic venous disease.
- Vein ablation treatments (eg Sclerotherapy, Radiofrequency or laser ablation, Vein ligation or stripping designed to destroy superficial veins that have abnormal valve function. These treatments are usually reserved for people with symptoms who do not respond to other treatments.
Page load link
 If the valves within the veins fail to work properly, blood can flow backwards in the veins and pool in the legs. The pooled blood can increase pressure in the veins.
If the valves within the veins fail to work properly, blood can flow backwards in the veins and pool in the legs. The pooled blood can increase pressure in the veins.